Technique to make CAR T-cells in vivo could transform cancer care Premium
The Hindu
Instead of extracting T-cells and engineering them in a lab, researchers have delivered mRNA directly into circulating immune cells, improving treatment outcomes and cutting the cost of CAR T-cell therapy.
In recent years, chimeric antigen receptor (CAR) T-cell therapy has changed outcomes for patients with aggressive blood cancers that no longer respond to standard treatments. In some acute leukaemias, CAR T-cell therapy has led to remissions lasting months or even years. Early-stage trials have explored its use in severe autoimmune diseases like lupus as well, where it may help reset a misfiring immune system.
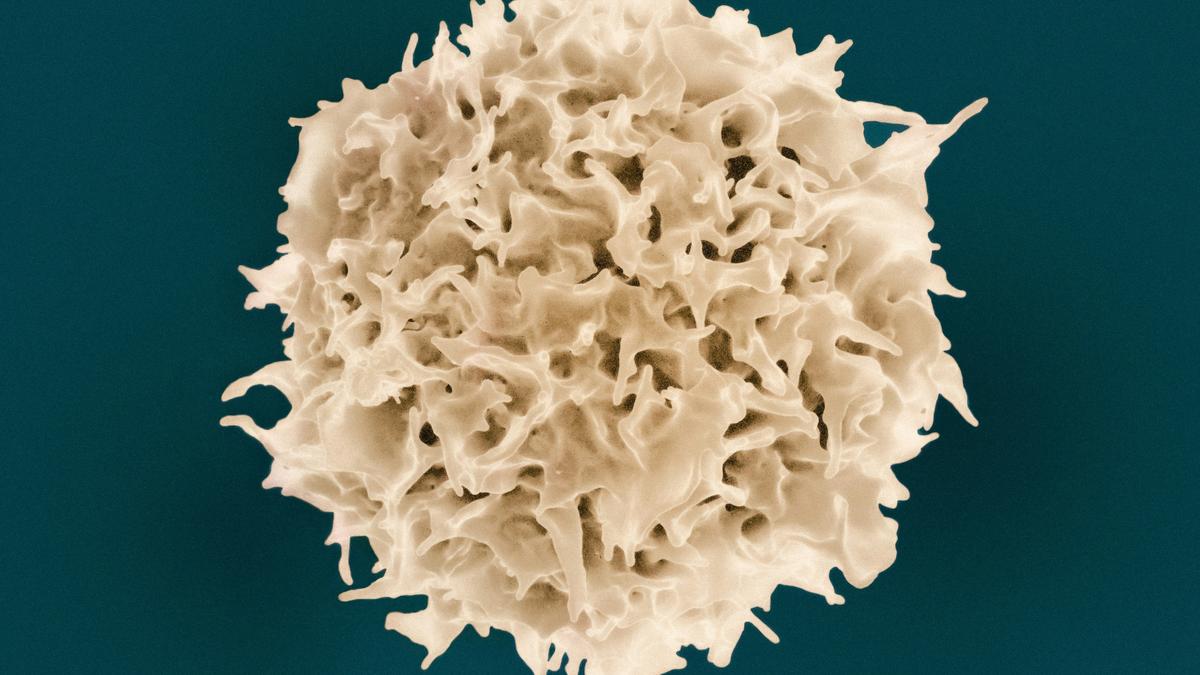
Originally developed in the early 1990s, the central idea behind CAR T-cell therapy is to retrain the body’s own immune cells to recognise and destroy rogue targets. T cells — the patrolling white blood cells — often fail to identify cancer cells. So scientists extract a patient’s T cells and insert genetic instructions that make them express the synthetic molecule, CAR. It gives T cells the ability to detect a specific ‘tag’ — most often CD19, which is found on nearly all B cells — that are the primary culprits in these cancers.
Once these reprogrammed T cells are infused back into the body, they expand, circulate, detect, and eliminate. The process is targeted and potent — but also slow, expensive, and complex. It requires personalised cell harvesting, lab-based genetic engineering using viral vectors, and chemotherapy to prepare the body to receive the modified cells.
Vishwanath S., a senior consultant in medical oncology, Apollo Hospitals, Bengaluru, estimated from personal practice that CAR T-cell therapy in India typically costs around ₹60-70 lakh. “Roughly ₹30-35 lakh goes toward manufacturing the personalised CAR T-cells through complex ex vivo processing,” he said. “The rest covers hospitalisation, supportive care, and monitoring for two to three weeks — including side effects, infections, and post-infusion care.”
A study in Science on June 19 by researchers from the US National Institute of Arthritis and Musculoskeletal and Skin Diseases, Capstan Therapeutics, and the University of Pennsylvania takes the core idea of CAR T-cell therapy and moves it entirely inside the body.
Instead of extracting T cells and engineering them in a lab, the researchers delivered messenger RNA directly into circulating immune cells using tiny, fat-based molecules known as lipid nanoparticles (LNPs). Commonly used in mRNA vaccines, they help genetic instructions enter target cells. To make sure the message reached the right cells, the researchers added a kind of biological address label: antibodies that bind specifically to CD8+ T cells, the immune system’s frontline killers. This targeted formulation, called a CD8-targeted lipid nanoparticle (CD8-tLNP) allowed the instructions to be delivered with precision.
When injected into mice, tLNPs carrying instructions for a CD19-targeting CAR successfully reprogrammed circulating CD8+ T cells, while in cynomolgus monkeys, a CD20-targeting version was used. Within days, B cells were depleted across multiple tissues, and tumours regressed in mice — all without personalised cell processing, viral vectors or chemotherapy. In monkeys, the treatment turned most CD8+ T cells (up to 85%) and nearly all related immune cells (95%) into cancer fighters after the second or third dose, showing strong results.













