From genomic medicine, a revolution rolls towards cancer care | Explained Premium
The Hindu
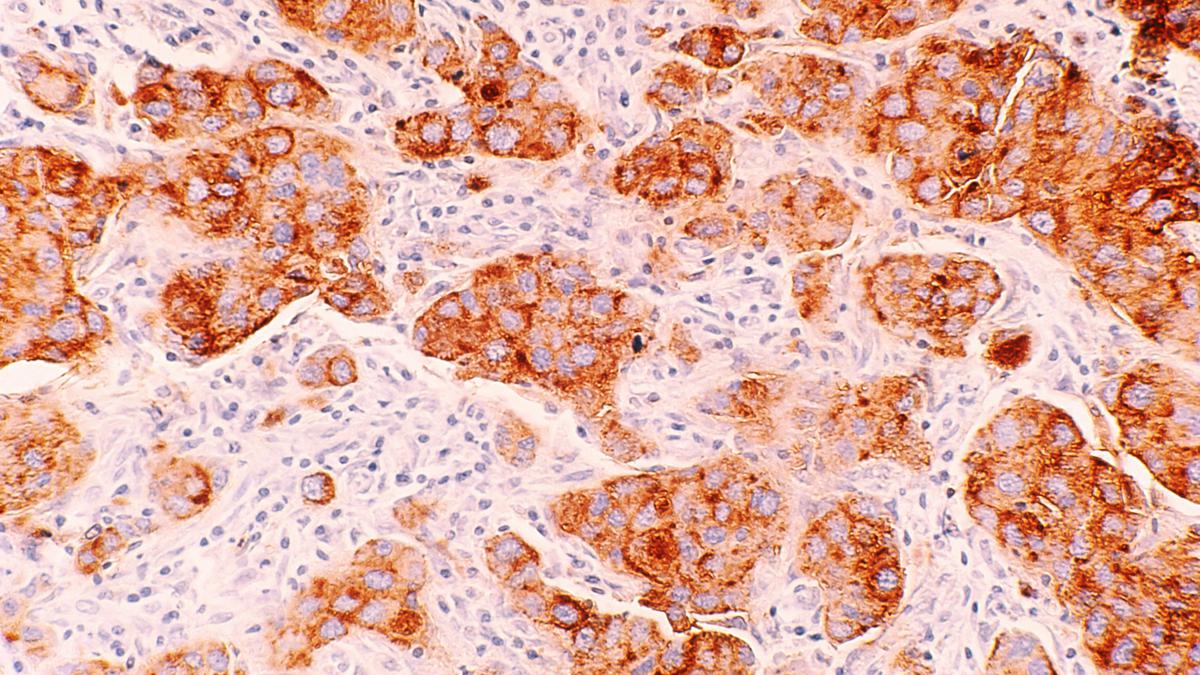
Cancer genomics has the potential to transform cancer care by providing personalised treatments based on genomic data.
Cancer has emerged as a major public health concern worldwide with about 20 million new patients being added every year. The World Health Organisation has estimated the cancer burden will increase by almost 60% over the next decade, potentially rendering it the second major cause of death. India alone adds approximately 1.4 million new cancer cases every year, with almost 1 in 1,000 Indians being diagnosed annually, per the National Cancer Registry.
Cancer is a disease of the genome. It is caused by changes in genes that cause some cells to divide in an uncontrolled way. These changes can be inherited or acquired. Inherited genetic variants form the basis of many hereditary cancers, including breast and ovarian cancer. Advancements in genomic technologies in the last couple decades, including global initiatives like the Cancer Genome Atlas, have provided a shot in the arm to understand the molecular underpinnings of cancer, which in turn have yielded a new generation of therapies that target molecular defects.
Such therapies are called precision oncology therapies. Their eligibility in a given setting is determined by molecular tests. Of the 200-odd therapies the U.S. Food and Drug Administration has approved, almost a third have a DNA-based test as biomarker. And while scientists are discovering new biomarkers for cancers, the focus of late has been shifting to understand how genomic tests could become the mainstay of cancer treatment in clinical settings.
As part of the U.K.’s ongoing ‘100,000 Genome Program’, a study of over 13,800 cancer patients, published last week, suggested cancer genomics could indeed transform cancer care. The programme reportedly demonstrated that genome sequencing integrated with routine clinical data could render cancer treatments more customisable. The implications of this study extend far beyond the boundaries of current practice of medicine, and mark a leap forward in the era of precision oncology.
At the heart of this transformation lies whole-genome sequencing (WGS), a tool that can sequence a person’s DNA in its entirety – i.e. all 3.2 billion nucleotides – in a single comprehensive test. The sequencing and in-depth analysis don’t treat the genome (derived from the blood) in isolation; instead, they happen together with the sequence of the genome obtained from cancerous tissue or a tumour.
In the U.K.-wide study, researchers obtained, sequenced, and analysed the genomes of people with different types of cancers; the genomes came from blood and tumour tissues. Their analysis revealed details that the researchers have said can be applied in clinical settings to guide treatment strategies for cancer patients.
Notably, according to the study, a higher fraction of individuals diagnosed with brain tumours as well as those dealing with bowel or lung cancers had distinct DNA changes that could become new targets for therapy. The study also provided novel insights that could reshape even our understanding of challenging conditions like ovarian cancers and sarcomas.

On January 11, 1922, 14-year-old Leonard Thompson became the first person to receive an insulin injection as a treatment for diabetes. A disease that had haunted humankind for millennia finally became treatable, and the century since has seen a lot happen, both good and bad. A.S.Ganesh takes stock of a disease that is now unfolding as a global epidemic…












